Introduction
You ask your autistic child to brush their teeth, something they’ve done hundreds of times before, and suddenly they’re running in the opposite direction, dissolving into distress, or becoming verbally combative. Five minutes later, unprompted, they head to the bathroom and brush their teeth perfectly well. What just happened?
If you’re parenting or working with autistic children, you’ve likely encountered this confusing pattern: an intense, anxiety-driven resistance to everyday demands and expectations that seems disproportionate to the request itself. This isn’t simple defiance, laziness, or bad behaviour. It’s a phenomenon increasingly recognised in autism research as demand avoidance.
But here’s where things get complicated. Demand avoidance in autism is one of the most debated, misunderstood, and emotionally charged topics in both clinical and community spaces. Some researchers and clinicians identify a distinct subtype called Pathological Demand Avoidance (PDA), whilst others view demand avoidance as a dimensional trait that exists across the autism spectrum. Meanwhile, parents are caught in the middle, desperately needing practical strategies whilst navigating conflicting professional opinions.
This post cuts through the confusion. We’ll examine what research actually tells us about demand avoidance in autism, explore competing frameworks, and most importantly, translate science into practical understanding. Because whether we call it PDA, demand avoidance, or something else entirely, the children experiencing it need our informed support.
What Is Demand Avoidance?
At its core, demand avoidance refers to an extreme anxiety-based need to avoid or resist everyday demands and expectations. But this simple definition conceals considerable complexity.
Beyond Typical Non-Compliance
All children resist demands sometimes. It’s a normal part of development and autonomy-seeking. Demand avoidance in autism is qualitatively different:
- Pervasive: It occurs across contexts (home, school, therapy, social situations) and with different people
- Anxiety-driven: The resistance stems from an overwhelming fight-or-flight response, not wilful defiance or desire to control
- Disproportionate: The intensity of the response far exceeds what the demand itself would typically warrant
- Impacts ordinary activities: Even pleasurable or self-initiated activities can trigger avoidance once they become an expectation
- Uses sophisticated strategies: Children may employ negotiation, distraction, excuse-making, or social manipulation to avoid demands
Importantly, demand avoidance often occurs even when the child wants to do the activity being requested. A child might desperately want to go to their friend’s birthday party but melt down when told it’s time to get ready to go. The expectation itself triggers the anxiety response.
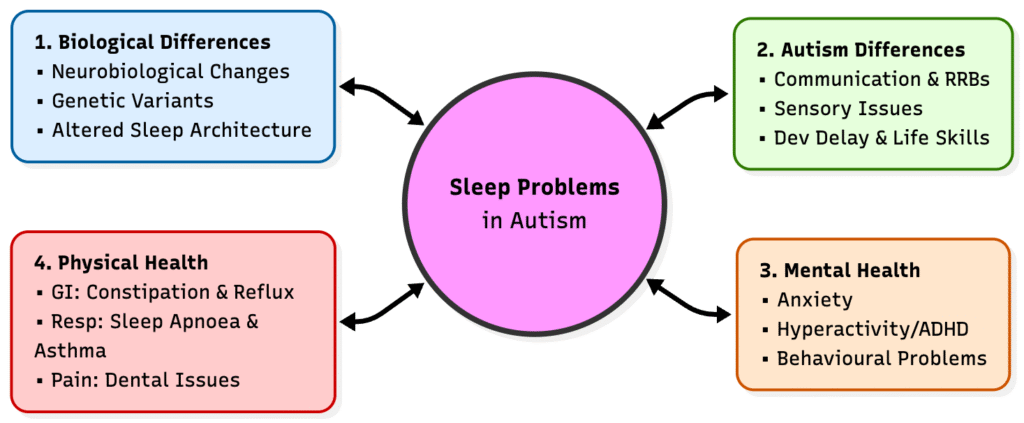
The Neurobiological Underpinnings
Whilst research is still evolving, several neurobiological factors likely contribute to demand avoidance:
Intolerance of uncertainty: Many autistic individuals experience heightened anxiety around unpredictability. Demands introduce uncertainty about what will happen, how long it will take, whether they’ll succeed, what comes next. The demand itself represents a loss of control over their immediate experience.
Executive function differences: Demands often require planning, task initiation, shifting between activities, and inhibiting current preferred activities. For autistic individuals with executive function challenges, demands represent a cognitive load that feels insurmountable, triggering threat responses.
Autonomy and control: Some researchers propose that demand avoidance relates to an unusually intense need to feel autonomous and in control of one’s experience. When external expectations are imposed, this threatens a core psychological need, activating defensive responses.
Nervous system dysregulation: For some autistic individuals, demands may more rapidly trigger autonomic nervous system responses (fight-flight-freeze), bypassing the cognitive processing that might allow for compliance.
The PDA Debate: One Profile or Many?
Here’s where clinical opinions diverge sharply, and understanding the debate helps parents and professionals make informed decisions about identification and support.
The PDA-as-Distinct-Profile View
First described by Elizabeth Newson in the 1980s, Pathological Demand Avoidance (note: many now prefer ‘Pervasive Drive for Autonomy’ to avoid stigmatising language) was proposed as a distinct profile within the autism spectrum characterised by:
- Extreme demand avoidance as the central difficulty
- Appearing socially comfortable on surface level, with better social mimicry than typical autism presentations
- Use of social strategies (negotiation, distraction, charm) to avoid demands
- Lability of mood, switching rapidly
- High levels of anxiety, particularly around loss of control
- Comfort in role play and pretend, but difficulty when play becomes structured
Proponents argue that PDA represents a meaningfully distinct presentation requiring specialised approaches. They point to clinical experience showing children who don’t respond to standard autism interventions but improve dramatically with PDA-informed approaches. Organisations like the PDA Society in the UK advocate for PDA recognition to ensure appropriate support.
Research status: PDA is not currently recognised in major diagnostic manuals (DSM-5 or ICD-11) as a separate condition. However, it has gained increasing recognition particularly in the UK, where some clinical services specialise in PDA identification and support.
The Dimensional-Trait View
Other researchers and clinicians view demand avoidance not as a distinct subtype but as a dimensional trait that exists along a continuum across the autism spectrum. In this framework:
- Demand avoidance varies in intensity from mild to extreme amongst autistic individuals
- It commonly co-occurs with particular profiles (high anxiety, strong need for control, executive function challenges)
- The specific features attributed to PDA (social strategies, role play) may simply reflect autistic individuals with relatively stronger social imitation skills who also happen to experience high demand avoidance
- Creating a separate PDA diagnosis may risk fragmentation and gatekeeping of support
Proponents argue that focusing on underlying needs (anxiety, autonomy, predictability) rather than categorical diagnosis allows for more flexible, individualised support without requiring a specific label.
What Does Research Show?
The evidence base remains limited, but growing:
Supporting distinction: Several studies have found that PDA questionnaires identify a cluster of children with distinct features from comparison autism groups, suggesting potential validity as a profile. Parent and clinician reports consistently describe a recognisable pattern.
Supporting dimensional view: Other studies find that demand avoidance behaviours exist on a continuum, with no clear categorical boundary separating PDA from high demand avoidance. Features attributed to PDA (like social strategies) correlate with other variables (like language ability) rather than forming a distinct syndrome.
The research consensus: Most researchers agree that extreme demand avoidance in autism is real, clinically significant, and requires specific approaches. Where they disagree is whether it constitutes a distinct condition or a dimensional trait. For parents and practitioners, this debate may be less important than understanding the underlying mechanisms and responding appropriately.
The Lived Experience: What Demand Avoidance Actually Looks Like
Understanding research frameworks matters, but translating this to real life is where parents and professionals need the most clarity. Demand avoidance manifests differently across ages, contexts, and individual profiles.
Early Childhood (Ages 2 to 5)
- Extreme distress at routine transitions: ‘Time for bath’ triggers immediate meltdown
- Physically fleeing or going limp when demands are introduced
- May appear compliant in novel situations (like first day at nursery) but struggles emerge as expectations become established
- Resists self-care tasks even when clearly uncomfortable (refuses coat in cold weather)
- May use early language to negotiate: ‘In a minute,’ ‘Not now,’ ‘Maybe later’
Common misinterpretations: ‘Terrible twos lasting years,’ ‘oppositional defiant disorder,’ ‘spoiled child who always gets their way’
Middle Childhood (Ages 6 to 11)
- Sophisticated avoidance strategies: bargaining, distraction, excuse-making, blaming others
- School refusal or extreme anxiety around school despite apparent social competence
- May appear socially engaged with peers but struggles intensify around structured activities
- Homework becomes a battleground, can take hours despite child clearly understanding content
- May achieve well in areas of special interest but shuts down completely for less preferred subjects
- Physical manifestations: stomach aches, headaches, feeling too tired when demands loom
Common misinterpretations: ‘Manipulative,’ ‘lazy,’ ‘capable when they want to be,’ ‘attention-seeking’
Adolescence (Ages 12 to 18)
- Demand avoidance may intensify as academic and social demands increase
- School dropout or persistent absence despite intellectual capability
- May struggle with basic self-care (showering, changing clothes) despite understanding importance
- Intense anxiety around future expectations (exams, university, employment)
- May express strong views about unfairness, rules, or others’ expectations
- Risk of withdrawal, depression, or mental health crisis as demands accumulate
Common misinterpretations: ‘Typical teenage rebellion,’ ‘oppositional defiant disorder,’ ‘depression’ (though depression may genuinely co-occur)
Across the Lifespan: Key Patterns
Regardless of age, certain patterns characterise significant demand avoidance:
The paradox of capability: Can complete complex tasks when self-initiated but cannot complete simple tasks when requested. Parents describe children who can build elaborate Minecraft worlds for hours but cannot write a three-sentence paragraph for school.
Masking and delayed collapse: May appear to cope in structured environments (school, therapy) through immense effort, then completely fall apart at home where they feel safe.
The request-distress cycle: Well-meaning adults increase demands or consequences in response to avoidance, which escalates anxiety and avoidance further, creating a vicious cycle.
Invisible anxiety: May not look anxious in conventional ways (no visible panic, may laugh or act silly) but are in genuine fight-or-flight mode internally.
Why Traditional Behavioural Approaches Often Backfire
Understanding demand avoidance becomes particularly important for intervention planning. Many children with significant demand avoidance have been through multiple rounds of behavioural interventions with limited success or even deterioration. Not because the interventions were poorly implemented, but because they fundamentally mismatched the child’s neurobiology.
The Standard Behavioural Model
Traditional behavioural approaches for non-compliance typically involve:
- Clear expectations and consistent consequences
- Reward systems for compliance
- Planned ignoring or removal of attention for avoidance
- Gradual increase in demands as child demonstrates capability
- Natural or logical consequences for continued refusal
These approaches rest on assumptions that non-compliance is maintained by reinforcement (attention, escape from tasks, access to preferred activities) and that altering contingencies will alter behaviour.
Why This Fails for Demand Avoidance
For children with anxiety-based demand avoidance, this model creates several problems:
It intensifies the threat response: More structure, clearer expectations, and consistent consequences increase predictability for some children but for those with demand avoidance, they increase the experience of demands (more things they have to do), triggering stronger anxiety and more desperate avoidance.
Rewards become demands: ‘If you do X, you get Y’ transforms the desired reward into a demand. The child now has to do X to get something they want, which triggers avoidance of both X and often Y as well.
It erodes trust and safety: Behavioural approaches require consistent implementation even when children are distressed. For demand-avoidant children in genuine fight-or-flight, this can feel like the safe adult is becoming a threat, damaging the relationship and increasing anxiety.
It targets behaviour, not underlying anxiety: Behavioural approaches aim to change the behaviour (compliance) but don’t address the anxiety driving avoidance. Even when compliance is achieved, anxiety remains or intensifies, often manifesting in other ways (self-harm, panic attacks, shutdown).
Natural consequences aren’t natural: For neurotypical children, experiencing consequences helps learning. For demand-avoidant children, consequences aren’t processed as learning opportunities. They’re additional threats confirming that the world is demanding and uncontrollable, reinforcing hypervigilance and defensive strategies.
What Research Shows About Behavioural Interventions
Studies examining outcomes of standard behavioural approaches for children with PDA or high demand avoidance show:
- Lower success rates compared to broader autism populations
- Risk of increased anxiety, aggression, or self-harm when demand pressure increases
- Parent reports using trauma language to describe behavioural programmes
- Better outcomes when approaches are modified to be low-demand and trust-based
This doesn’t mean behavioural principles are irrelevant. Understanding what maintains behaviour remains valuable. But the application must account for anxiety-driven demand avoidance rather than treating it as operant non-compliance.
Evidence-Based Approaches: The Low-Demand, High-Trust Framework
So if traditional approaches often fail, what does work? Research and clinical experience increasingly point towards low-demand, trust-based approaches that prioritise nervous system regulation and autonomy before compliance.
Core Principles
1. Reduce overall demand load
The fundamental starting point is reducing the total number of demands and expectations in the child’s environment. Not as a reward for behaviour, but as an environmental modification to reduce nervous system activation.
This means:
- Identifying and eliminating non-essential demands
- Reducing demands during high-stress periods (transitions, illness, environmental changes)
- Recognising that everything can feel like a demand: questions, praise, even offers of help
2. Prioritise trust and connection over compliance
When forced to choose between maintaining a trusting relationship and enforcing compliance with a demand, choose relationship every time. A child in fight-or-flight around demands cannot learn, develop skills, or internalise values. They’re simply surviving. A child who trusts their adult and feels safe can gradually build capacity.
3. Collaborate rather than direct
Shift from ‘I need you to do X’ to ‘We have this challenge; what ideas do you have?’ Genuine collaboration restores agency and reduces the experience of imposed demands.
4. Offer choice and control wherever possible
Even tiny choices help: ‘Would you like to brush your teeth before or after pyjamas?’ ‘Should I set a five-minute or ten-minute timer?’ ‘Do you want company or alone time for this?’
5. Declarative language over imperatives
Replace direct demands with observations or shared problem-solving:
- Instead of: ‘Put your shoes on now’
- Try: ‘I notice it’s nearly time to leave. I’m wondering about shoes.’
This approach invites collaboration rather than triggering resistance.
6. Flexible boundaries, not rigid rules
Safety boundaries remain non-negotiable, but flexibility around methods, timing, and implementation reduces demand experience. The goal is achieved differently rather than not at all.
Practical Implementation Strategies
Indirect approaches: Rather than direct requests, create situations where the desired outcome happens without explicit demands. Leave toothbrush visible, model tooth-brushing yourself, mention casually ‘My teeth feel so clean now,’ then give space.
Humour and playfulness: Turning demands into games, using silly voices, or approaching tasks obliquely through imagination can bypass demand-resistance. ‘I wonder if the toothbrush can reach alllll the way to the back teeth!’
Role play and identity: Many demand-avoidant children respond better when acting as a character or helping someone else. ‘Can you show teddy how to brush teeth?’ feels different than ‘Brush your teeth.’
Clear information without obligation: Provide information that allows autonomous decision-making: ‘Dentist appointment is at 3pm. The car leaves at 2:45,’ then step back. You’ve informed without demanding.
Careful praise: Some demand-avoidant children experience praise as pressure or implied expectation. Notice and appreciate without evaluating: ‘You did it’ rather than ‘Good job’ or ‘I’m proud of you.’
Energy accounting: Recognise that compliance costs enormous energy. Pick your battles ruthlessly. Does this demand genuinely matter right now, or is it negotiable?
What Does the Evidence Say?
Research on low-demand approaches is emerging:
- Clinical case studies and parent reports consistently describe dramatic improvements when approaches shift to low-demand frameworks
- Qualitative research with PDA-identified individuals emphasises the importance of autonomy, collaboration, and reducing demand pressure
- Preliminary quantitative studies suggest reduced parental stress and improved child wellbeing with PDA-informed approaches
- No studies show harm from low-demand approaches, whilst concerning outcomes are documented from high-structure behavioural approaches
However, we need more rigorous controlled research comparing different approaches systematically.
Addressing Common Concerns and Misconceptions
Inevitably, low-demand approaches raise concerns from educators, clinicians, and even parents themselves. Let’s address these directly.
‘Aren’t we just giving in? Won’t this create an entitled, manipulative child?’
This concern rests on the misunderstanding that demand avoidance is wilful control-seeking rather than anxiety-driven. Consider:
- Children don’t want to avoid demands. They experience unbearable anxiety when demands occur
- These children are often desperately unhappy with their own avoidance patterns
- Building capacity requires first reducing nervous system activation; teaching happens from a foundation of safety, not during crisis
- Low-demand approaches are temporary scaffolding, not permanent accommodation. As nervous system regulation improves and trust builds, capacity gradually increases
Research note: Studies consistently show that children with PDA experience high levels of anxiety and often depression. This isn’t consistent with ‘getting their way’. It’s consistent with chronic nervous system dysregulation.
‘But they need to learn compliance for the real world’
This argument assumes that forcing compliance now teaches compliance later. Research and lived experience suggest otherwise:
- Forced compliance during high anxiety teaches that the world is threatening and adults can’t be trusted, increasing defensiveness
- Many demand-avoidant individuals who receive low-demand support in childhood develop better adult functioning than those subjected to forced compliance
- Real-world demands in adulthood often come with more autonomy, choice, and control than childhood demands. Many adults with demand avoidance profiles function well in self-directed careers
The goal isn’t avoiding all demands forever. It’s building capacity gradually from a foundation of trust and nervous system regulation.
‘How do we keep them safe if we can’t make demands?’
Safety isn’t negotiable, but how we ensure safety can be flexible:
- Safety boundaries can be maintained through environmental modification rather than constant verbal demands
- Collaboration on safety plans when the child is regulated
- Focusing on relationship and trust so that when genuine safety demands occur, the child’s nervous system doesn’t immediately escalate
- Recognising that forced compliance around non-safety issues erodes trust and makes safety compliance less likely
‘What about education? They need to learn things’
Absolutely, but learning requires a regulated nervous system. A child in fight-or-flight cannot encode new information effectively. Consider:
- Children with demand avoidance often teach themselves complex topics independently when not framed as demands
- Interest-led, autonomy-supportive education often results in deep learning
- Academic outcomes for PDA children in traditional schooling are often poor despite intelligence; alternative approaches show better results
- Short-term academic falling behind during high-anxiety periods is preferable to long-term school refusal, trauma, or mental health crisis
Moving Forward: Research Gaps and Clinical Needs
Despite growing recognition, demand avoidance in autism remains significantly under-researched. Important gaps include:
Research Priorities
Diagnostic clarity: We need consensus on whether PDA or demand avoidance represents a distinct condition, a dimensional trait, or multiple subtypes. Current diagnostic uncertainty creates barriers to accessing appropriate support.
Longitudinal studies: How does demand avoidance change across development? What factors predict better or worse outcomes? What are the long-term effects of different intervention approaches?
Neurobiological research: What underlying neurobiology drives demand avoidance? Brain imaging, physiological measurement, and genetic research could clarify mechanisms.
Intervention trials: Rigorous comparison of low-demand versus traditional behavioural approaches, with careful attention to outcomes beyond just compliance (anxiety, quality of life, mental health, long-term functioning).
Adult outcomes: Most research focuses on children. What happens to demand-avoidant autistic individuals in adulthood? How can we support successful transition to independence?
Cultural considerations: Nearly all current research comes from the UK. How do cultural factors influence the expression and recognition of demand avoidance?
Clinical and Educational Needs
Professional training: Most clinicians and educators haven’t received training in recognising or supporting demand avoidance, leading to misdiagnosis and inappropriate interventions.
Service accessibility: In regions where PDA is recognised, assessment waitlists can be years long. Where it’s not recognised, families struggle to access any specialised support.
School accommodations: Educational systems need clearer frameworks for supporting demand-avoidant students that go beyond standard autism or behavioural support plans.
Family support: Parents of demand-avoidant children experience exceptional stress and often face judgement from professionals and family members. They need specialised parent education and mental health support.
Conclusion: From Debate to Support
Whether we ultimately define demand avoidance as a distinct syndrome, a dimensional trait, or something else entirely matters less than this: children with extreme anxiety-driven demand avoidance are real, their struggles are profound, and they need our informed, compassionate support.
The evidence increasingly suggests that these children don’t respond well to approaches that work for other children. Not because they’re more difficult or manipulative, but because their neurobiology creates different needs. Low-demand, trust-based, autonomy-supportive approaches show the most promise, even as we need more rigorous research.
For parents reading this: trust your instincts. If traditional approaches haven’t worked, if your child seems more anxious rather than less, if you feel you’re losing your relationship in pursuit of compliance, you’re not imagining it. Seek clinicians and educators familiar with demand avoidance, advocate for low-demand approaches, and know that your child’s resistance isn’t wilful opposition. It’s a nervous system crying out for safety, autonomy, and understanding.
For professionals: stay curious. When a child doesn’t respond to evidence-based interventions that work for most autistic children, consider whether demand avoidance might be a factor. Be willing to radically shift your approach, prioritise trust over compliance, and recognise that behavioural doesn’t always mean the same intervention fits all presentations.
The research on demand avoidance in autism is evolving rapidly. We don’t have all the answers yet. But what we know already is enough to transform how we support some of our most anxious, misunderstood autistic children. That transformation is long overdue.
Research References and Further Reading
Foundational PDA Literature
Newson, E., Le Maréchal, K., & David, C. (2003). Pathological demand avoidance syndrome: A necessary distinction within the pervasive developmental disorders. Archives of Disease in Childhood, 88(7), 595-600. https://adc.bmj.com/content/88/7/595
This seminal paper introduced PDA as a distinct profile within the autism spectrum.
O’Nions, E., Christie, P., Gould, J., Viding, E., & Happé, F. (2014). Development of the ‘Extreme Demand Avoidance Questionnaire’ (EDA-Q): Preliminary observations on a trait measure for pathological demand avoidance. Journal of Child Psychology and Psychiatry, 55(7), 758-768. https://acamh.onlinelibrary.wiley.com/doi/10.1111/jcpp.12149
Development of a measure to assess PDA features, providing tools for research and clinical identification.
Christie, P., Duncan, M., Fidler, R., & Healy, Z. (2011). Understanding Pathological Demand Avoidance Syndrome in Children: A Guide for Parents, Teachers and Other Professionals. Jessica Kingsley Publishers.
A comprehensive clinical guide covering identification and management strategies.
Recent Research on PDA and Demand Avoidance
O’Nions, E., Viding, E., Greven, C. U., Ronald, A., & Happé, F. (2014). Pathological demand avoidance: Exploring the behavioural profile. Autism, 18(5), 538-544. https://journals.sagepub.com/doi/10.1177/1362361313481861
Examined behavioural characteristics distinguishing PDA from broader autism.
Stuart, L., Grahame, V., Honey, E., & Freeston, M. (2020). Intolerance of uncertainty and anxiety as explanatory frameworks for extreme demand avoidance in children and adolescents. Child and Adolescent Mental Health, 25(2), 59-67. https://acamh.onlinelibrary.wiley.com/doi/10.1111/camh.12336
Investigated intolerance of uncertainty as a mechanism underlying demand avoidance.
Truman, C., Teague, S. J., & Maybery, M. (2021). Testing the construct validity of proposed pathological demand avoidance behaviours. Research in Developmental Disabilities, 112, 103913. https://www.sciencedirect.com/science/article/abs/pii/S0891422221000317
Recent examination of whether PDA behaviours constitute a distinct construct.
Curtis S, Izett E.. (2025).
The experience of mothers of autistic children with a pathological demand avoidance profile: an interpretative phenomenological analysis. Discov Ment Health. 2025 Jan 20;5(1):5. doi: 10.1007/s44192-025-00127-3. PMID: 39833592; PMCID: PMC11747059.
The lived experiences of parents raising a child with pathological demand avoidance.
Green, J., Absoud, M., Grahame, V., et al. (2018). Pathological demand avoidance: Symptoms but not a syndrome. The Lancet Child & Adolescent Health, 2(6), 455-464. https://www.thelancet.com/journals/lanchi/article/PIIS2352-4642(18)30044-0/fulltext
Critical examination of PDA as a distinct syndrome versus symptom cluster.
Gillberg, C., Gillberg, I. C., Thompson, L., Biskupsto, R., & Billstedt, E. (2015). Extreme (‘pathological’) demand avoidance in autism: A general population study in the Faroe Islands. European Child & Adolescent Psychiatry, 24(8), 979-984.
Population-based study examining prevalence and characteristics.
Kildahl, A. N., Helverschou, S. B., Rysstad, A. L., Wigaard, E., Hellerud, J., Ludvigsen, L., & Howlin, P. (2021). Pathological demand avoidance in children and adolescents: A systematic review. Autism, 25(8), 2162-2176. https://journals.sagepub.com/doi/10.1177/13623613211012611
Recent systematic review synthesising current evidence on PDA.
Intervention and Support Approaches
Milton, D., Mills, R., & Pellicano, E. (2014). Ethics and autism: Where is the autistic voice? Commentary on Post et al., Journal of Autism and Developmental Disorders, 44, 2650-2651.
Important perspective on involving autistic voices in research and practice.
Fisher, P., Goodley, D., & Lawthom, R. (2021). From pathology to public health: Reconceptualising pathological demand avoidance. Autonomy, the Critical Journal of Interdisciplinary Autism Studies, 1(7).
Critical analysis advocating for reconceptualisation of PDA.
Gore Langton, E., & Frederickson, N. (2016). Mapping the educational experiences of children with pathological demand avoidance. Journal of Research in Special Educational Needs, 16(4), 254-263. https://nasenjournals.onlinelibrary.wiley.com/doi/abs/10.1111/1471-3802.12073
Examination of educational approaches and outcomes for children with PDA.
Fidler, R., & Christie, P. (2019). Collaborative approaches to learning for pupils with PDA: Strategies for Education Professionals. Jessica Kingsley Publishers.
Practical guide for educational settings informed by clinical experience.
Critical Perspectives and Debates
Reilly, C., Atkinson, P., Menlove, L., Gillberg, C., O’Hare, A., Baird, G., Absoud, M., et al. (2020). Pathological demand avoidance: Descriptive and diagnostic considerations. Research in Developmental Disabilities, 101, 103654.
Discussion of diagnostic considerations and challenges.
Gillberg, C. (2014). Commentary: PDA, public display of affection or pathological demand avoidance? Journal of Child Psychology and Psychiatry, 55(7), 769-770.
Commentary on the PDA construct and its validity.
Resources for Families and Professionals
PDA Society (UK): https://www.pdasociety.org.uk Leading charity providing information, support, and resources for families and professionals.
PDA Resource: http://www.pdaresource.co.uk Educational resource site offering practical strategies and training.
National Autistic Society (PDA Profile): https://www.autism.org.uk/advice-and-guidance/what-is-autism/pda Information and guidance on the PDA profile within autism.
PDA North America: https://pdanorthamerica.org Resources and community for North American families and professionals.
Note: This is an evolving area of research. New studies are being published regularly. For the most current research, search databases like PubMed, PsycINFO, and Google Scholar using terms: ‘pathological demand avoidance,’ ‘extreme demand avoidance,’ ‘PDA autism,’ and ‘demand avoidance profile.’